Malaria in 2025 - Progress, Pressure & A Turning Point
The World Malaria Report 2025, released by the World Health Organization (WHO), arrives at a moment of both progress and growing concern. While global interventions continue to expand and new tools are making measurable impact, the world is also facing rising cases, widening financial gaps and an unprecedented threat from drug-resistance. Together, these forces signal that the fight against malaria is entering a new phase—more advanced than before, but also more fragile.
A Global Burden That Isn’t Falling Fast Enough
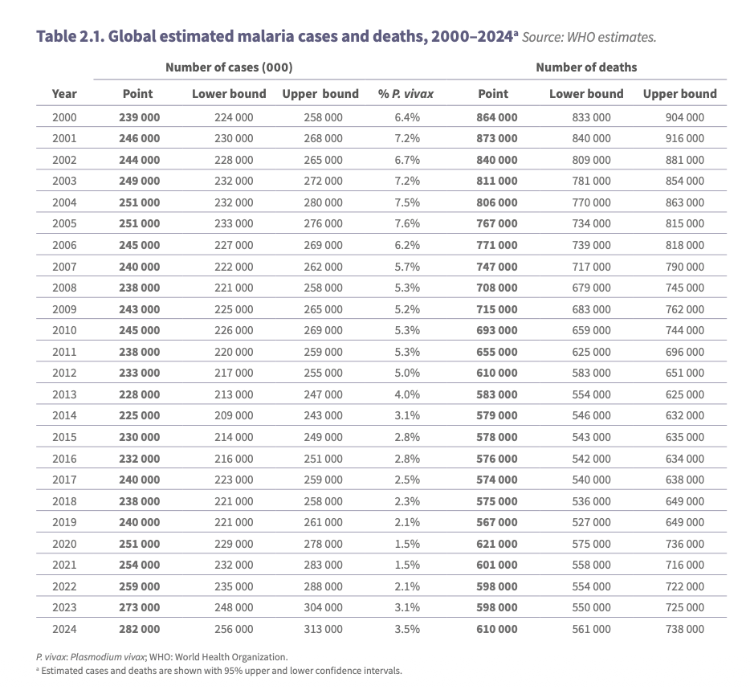
In 2024, an estimated 282 million malaria cases were recorded worldwide—an increase of around three percent from the previous year. More than 600,000 deaths were reported, the majority among young children. The increase in cases was driven largely by countries experiencing conflict or severe climate threats. Ethiopia, Madagascar and Yemen alone accounted for more than half of the global rise, showing just how closely malaria outcomes are now tied to political instability, environmental disruption and weakened health systems.
Although these numbers are concerning, they do not reflect failure. Rather, they illustrate how complex malaria control has become. As climate pressures intensify and conflict zones expand, malaria is increasingly exploiting gaps beyond traditional public-health challenges.
Progress Worth Noticing
At the same time, there are clear signs of forward movement. WHO estimates that more than a million deaths were averted in 2024, as improved prevention tools, increased chemoprevention, strengthened surveillance and targeted programming reached more communities. Several countries continue to prove that elimination is possible. Cabo Verde and Egypt were certified malaria-free in 2024, followed by Georgia, Suriname and Timor-Leste in 2025. These successes demonstrate that with long-term commitment, effective control strategies and reliable financing, malaria elimination is achievable—even in former high-burden settings.
The report also notes the gradual expansion of immunisation in some settings, but importantly, prevention and treatment tools outside vaccination remain the primary drivers of reduced mortality and transmission in most high-burden areas. Interventions such as chemoprevention, insecticide-treated nets, and rapid diagnosis remain central pillars of malaria control efforts.
Drug Resistance: The Most Critical Emerging Threat
This year’s report places serious emphasis on the spread of antimalarial drug resistance. Partial resistance to artemisinin, the core component of global treatment, has now been confirmed or suspected in multiple African countries. Even more concerning are early signs that partner drugs used alongside artemisinin may also be declining in effectiveness, raising the possibility of treatment failures in the future. Simultaneously, genetic shifts within the parasite population are reducing the reliability of rapid diagnostic tests in certain regions, while resistance to insecticides continues to limit the effectiveness of vector control tools.
If not addressed urgently, resistance could reverse years of progress and undermine some of the most successful malaria strategies ever implemented. This is arguably the most significant threat identified in the 2025 report.
A Rising Burden and Shrinking Resources
A particularly urgent concern is funding. In 2024, global malaria financing met only 42% of what is required to stay aligned with internationally agreed reduction targets. The report warns that sudden cuts in international health assistance during 2025 have already disrupted prevention and treatment services in high-burden regions. In some countries, shortfalls have led directly to medicine shortages, delayed campaigns and reduced household access to care. Unsurprisingly, the consequences fall heaviest on children and on communities already experiencing conflict or climate emergency.
What Happens Next
Despite the challenges, the overall message is clear: the world has the tools needed to move from malaria control toward genuine elimination. However, doing so will require faster rollout of proven interventions, investment in resistance-resilient solutions, and stronger domestic leadership in high-burden regions. The next decade, more than any period before, will determine whether malaria continues its slow decline or whether resistance and financial strain push global progress backward.
Our Response
At Landcent, we recognise that this new phase demands innovation focused on resilience, solutions that remain effective even as resistance grows and funding becomes unpredictable. We are advancing next-generation prevention technologies, developing tools specifically designed for low-resource settings, and supporting strategies that strengthen long-term control while building a foundation for eventual elimination.
This fight is changing, and the tools must change with it. Landcent remains committed to driving accessible, affordable and sustainable solutions—because malaria won’t wait, and neither will we.
More Updates
Subscribe to The Newsletter
Be the first to know—Get the latest news, discoveries, and impact stories that matter


%204.png)





